 Fast heart rates arising from the lower chambers of the heart (ventricles) can cause the heart to beat abnormally resulting in a lack of blood flow to the brain resulting in fainting or sudden death. These rhythms are often due to ventricular fibrillation or ventricular tachycardia. Once these rhythms begin it is crucial to restore normal beating and thus restore blood flow to the brain. With every passing minute, brain damage or death becomes increasingly more likely. A defibrillator or ICD (Implantable Cardiovertor Defibrillator) can detect the onset of these rhythms and shock the heart within seconds of its onset and thereby save the life of the patient and/or markedly reduce the likelihood of brain damage.
Fast heart rates arising from the lower chambers of the heart (ventricles) can cause the heart to beat abnormally resulting in a lack of blood flow to the brain resulting in fainting or sudden death. These rhythms are often due to ventricular fibrillation or ventricular tachycardia. Once these rhythms begin it is crucial to restore normal beating and thus restore blood flow to the brain. With every passing minute, brain damage or death becomes increasingly more likely. A defibrillator or ICD (Implantable Cardiovertor Defibrillator) can detect the onset of these rhythms and shock the heart within seconds of its onset and thereby save the life of the patient and/or markedly reduce the likelihood of brain damage.
Patients who are at risk for these rhythms typically have very weak hearts and have never experienced a ventricular rhythm problem. Other patients have genetic abnormalities which leave them at risk due to structural problems with the heart or problems with how the heart handles electrolytes. Your cardiologist can determine whether or not you would benefit from a defibrillator.
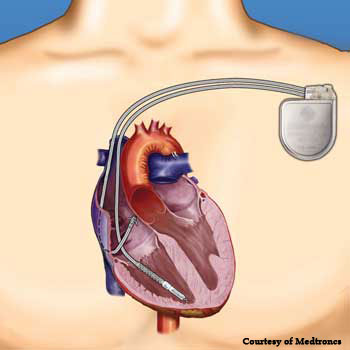 Defibrillators are small devices that are placed under the skin just below the collarbone similar to a pacemaker. Like a pacemaker, the defibrillator can pace the heart during slow rhythms but in addition it can shock the heart out of very fast rhythms. When the heart rhythm is normal, the defibrillator does nothing except monitor the heart.
Defibrillators are small devices that are placed under the skin just below the collarbone similar to a pacemaker. Like a pacemaker, the defibrillator can pace the heart during slow rhythms but in addition it can shock the heart out of very fast rhythms. When the heart rhythm is normal, the defibrillator does nothing except monitor the heart.
The operation is almost identical to a pacemaker placement and typically takes 30-60 minutes. It is performed under local anesthesia with mild to moderate sedation but not general anesthesia. (General anesthesia will increase the risk for complications with the procedure). Typically the only discomfort felt is during the injection of local anesthesia at the start of the procedure. A small incision is made under the clavicle and a wire is placed through the vein below the collarbone into the heart (right ventricle). The small generator is then placed under the skin and attached to the wire. You will spend the night in the hospital the night after the procedure on a cardiac unit. A chest x-ray will be performed the following day and typically the patient is discharged to follow-up our Device Clinic as well as with your cardiologist.
Periodically (typically once a year), we will check the device function to make sure that it is functioning appropriately. This procedure typically takes a couple of hours and does not require an admission to the hospital. During the procedure the patient is placed briefly under general anesthesia and the device will be programmed to initiate an arrhythmia which it will then automatically detect and terminate. One of our cardiologists will be present assessing the device function and will make any adjustments in the device settings if needed. After the assessment, the patient can go home and resume normal activities without any new restrictions.
In 2007, Merrimack Valley Cardiology became the only cardiology group in the area that specializes in placing and managing these devices. By developing a local electrophysiology program, we are bringing these increasingly common and safe procedures to the community and improve the overall cardiovascular care of our patients.
What to Expect Before the Procedure:
- Nothing to eat after the midnight before the procedure.
-
- You may take your pills with small sips of water.
- Diabetes pills should be held and if you take insulin, ask your physician how the dose should be adjusted.
- If you take Coumadin, aspirin or Plavix, please ask your cardiologist if these should be withheld before the procedure.
- You may bring a CD of your favorite music to help you relax.What to Expect After the Procedure:
- There may be soreness at the incision site and possibly some swelling and bruising.
- The dressing should be left in place for 3 days.
- You should not take a shower for at least 3 or 4 days and definitely not bathe or swim for several weeks.
- You should try to limit large motions of the affected arm to avoid pulling out one of the wires before it has fully healed.
- Ask your cardiologist when you can drive.
- Follow up in the Device Clinic will be arranged for approximately one week to check the wound and evaluate the pacemaker or defibrillator function. There will not be any external stitches to remove, although occasionally the cardiologist may use staples which will require removal.
Complications:
Possible complications of the surgery are infection, collapse of a lung, perforation of the heart and excessive bleeding. Your cardiologist is trained in managing these potential complications.
For more information about Defibrillators, click here.
